Matrix, reprogrammed: overcoming melanoma relapse
Cornell researchers discovered how the extracellular matrix (ECM), the supportive scaffold that surrounds every cell in the body, contributes to cancer therapy effectiveness. In a paper published in Advanced Science in August 2025, they show that the ECM changes that appear during melanoma treatment and lead to treatment resistance can be reversed with drugs that reduce the ECM density, opening new therapeutic directions.
“Melanoma patients usually respond very well to targeted therapy at first, but most eventually relapse as their tumors become resistant to treatment,” says Dr. Andrew White, associate professor in the Department of Biomedical Science and senior author of the study. “We wanted to understand what causes this resistance.”
The ECM caught the team’s attention because they noticed striking changes in collagen, the main structural protein of the ECM, during treatment: the ECM becomes unusually dense and overproduced. “What we wanted to know is whether the changes in the ECM were just a side effect of therapy, or if they actually contributed to drug resistance,” said Chia-Hsin Hsu, graduate student and first author of the study.
The team made two discoveries. First, they explained why even the most powerful targeted therapeutics can fail: they showed that the thickened matrix acts like a physical barrier, preventing cytotoxic T cells, the immune cells that directly kill cancer, from reaching the tumor. “It changes the way we think about cancer treatment, from focusing only on the cancer cells themselves to understanding and treating the entire tissue environment around them,” Hsu said.
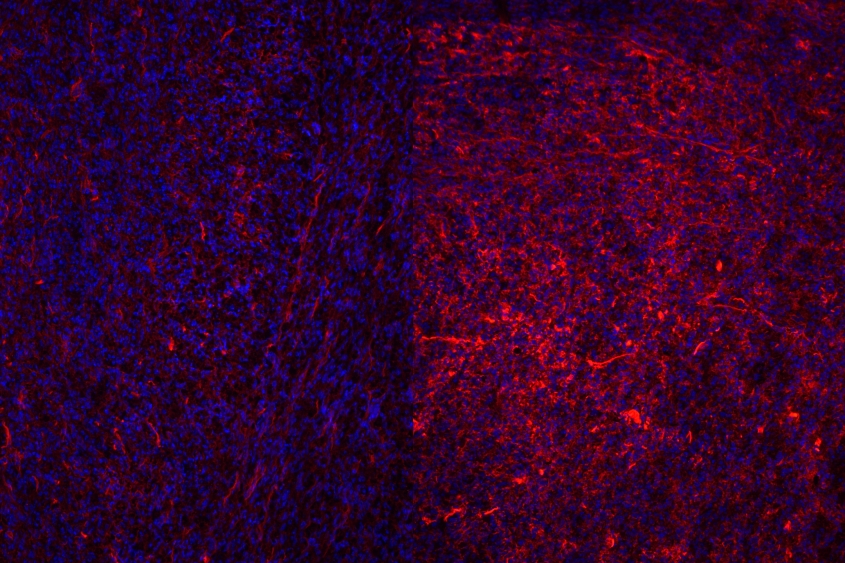
Second, using drugs that reduced or loosened this matrix allowed T cells re-enter the tumor and attack the tumor again. “It was thrilling to see how changing the extracellular matrix (ECM) could completely reshape the immune landscape of a tumor. Under the microscope, we could literally see cytotoxic T cells spreading more evenly once the ECM was reduced. It felt like uncovering a hidden mechanism that had been holding back the immune system from doing its job,” Hsu said.
According to the researchers, the discovery could lead to new treatments, pairing existing targeted drugs or immunotherapies with agents that modify the extracellular matrix. Some of these ECM-modifying drugs already exist and are being tested for tissue scarring. Repurposing or fine-tuning them for cancer could help prevent relapses or make existing treatments more effective.
The team is now investigating whether ECM molecules other than collagen affect therapy resistance, and if targeting these molecules could reshape the tumor microenvironment more broadly and further help overcome resistance to therapy.
“Therapy doesn’t happen in isolation; it takes place within the constantly changing ecosystem of the tumor microenvironment, and the extracellular matrix is a vital part of that ecosystem,” Hsu said. “Our study reminds us that curing cancer isn’t just about killing cancer cells; it’s also about restoring the body’s own environment so that the immune system can fight back effectively.”
A version of this story is published in the Cornell Chronicle