New study emphasizes importance of partnerships when conducting surveillance surveys
Early in the COVID-19 pandemic, the prevalence of cases was determined by how many people were testing positive every day, using PCR tests. While the tests themselves are considered highly accurate, there were limitations to this method, as not everybody had the same access to testing, and those with asymptomatic infections were unlikely to seek out a test.
In February, April and October of 2022, The Cazer lab at Cornell University, in partnership with Tompkins County Public Health department and Cayuga Health System, surveyed three municipalities in Tompkins County, using a two-stage cluster sampling model developed by researchers at Oregon State University.
The findings were published in the Jan. 29 issue of AJPM Focus. They confirmed that door-to-door surveillance surveys — which collect information from households or individuals in a specific geographical area — can often provide more precise estimates of how many people are infected with COVID-19 or have immunity to COVID-19 at any given point in time.
Getting to the gold standard
However, while surveillance studies are often considered the gold standard for collecting reliable data, they can be labor- and resource-intensive. The researchers emphasized the importance of leveraging existing relationships with institutions, thoroughly and consistently training volunteers, and creating new partnerships to make this method more efficient and sustainable.
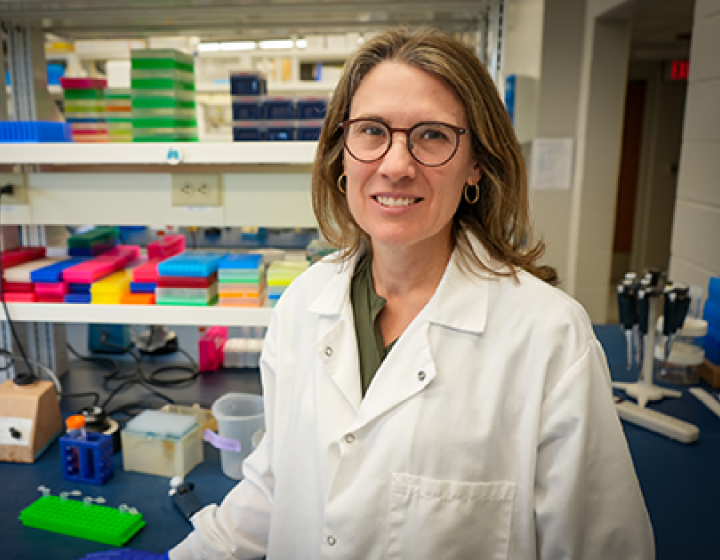
“Some of the things that contributed to our success were the fact that we had really strong partnerships with the Tompkins County Health Department and Cayuga Health System,” says Casey Cazer, D.V.M. ’16, Ph.D. ’20, lead author of the study. Cazer is an assistant professor in the Department of Clinical Sciences and the Department of Public and Ecosystem Health, as well as the associate hospital director of the Small Animal Community Practice Service in the College of Veterinary Medicine.
“Because of those partnerships, we were able to use existing infrastructure and tools," Cazer says. "So, we were able to run our COVID tests through the Cornell COVID-19 Testing Lab, which was a partnership with Cayuga Health System, and we were able to use existing technology systems from the Cayuga Health System to de-identify our samples and enable us to collect anonymous information."
Cazer's team also leveraged the training methodology their partners at Oregon State University had used, combining that with Cornell's existing training for key steps such as handling infectious samples. "Putting together a combination of borrowed and new training helped our team members be successful," she says.
Using census blocks, the teams randomly chose different areas to sample, and surveyed one municipality at a time. Cazer said the student volunteers would knock on every 10th door (approximately) and ask people if they wanted to participate in the study and give a sample.
Participants provided self-administered nasal swabs, which were tested for the virus as well as for antibodies. They also provided demographic information, symptom history, and vaccination status, and answered questions on COVID-19 prevention behaviors and attitudes. All in all, 233 individuals were sampled. The response rate ranged from 39% to 46%.
Understanding uncertainty
Cazer says the results showed a high level of asymptomatic infections “We found that some people had antibodies from a previous infection, but they did not report ever having a positive COVID test. It’s not surprising, but it confirms that there was a large amount of asymptomatic spread.”
The team hopes that the surveillance surveys provided timely and reliable evidence to inform local public health officials’ decision-making efforts in response to the COVID-19 pandemic. They encourage other universities or health departments that might want to do this kind of work to increase their odds of success by leveraging existing partnerships and tools.
Cazer’s team is currently collaborating with members of Cornell's School of Operations Research and Information Engineering to understand how uncertainty impacts epidemiologic models of pandemics. “There were a lot of different models and forecasts available of what was going to happen with COVID-19,” Cazer says. “Because there were limited amounts of information available, sometimes those models were not very accurate. We're interested in trying to understand how that sort of uncertainty about what's happening in real time impacts our ability to forecast those diseases and will help us to develop better forecasts for the next pandemic.”
Written by Christina Frank