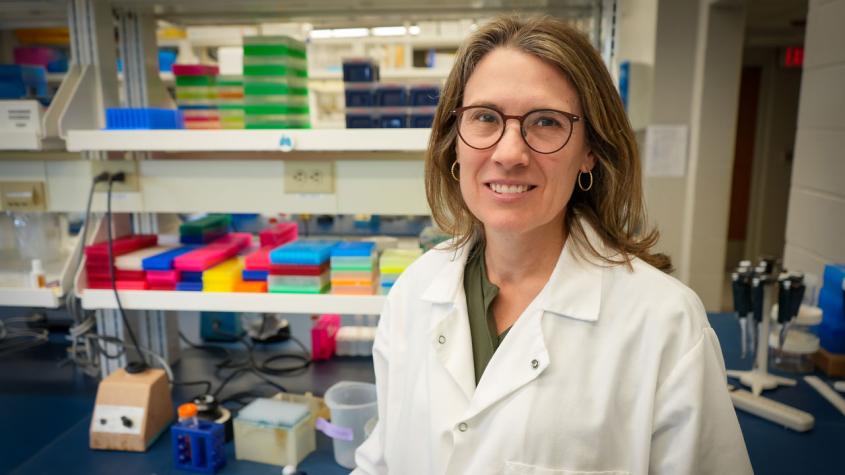
New faculty profile: Dr. Mandi de Mestre
The Cornell University College of Veterinary Medicine (CVM) has recently welcomed many new faculty members to our academic departments and hospitals, each one bringing a unique set of skills and experience that enriches our college every day. In this Q&A series, you'll get to know their interests, expertise and more.
Dr. Mandi de Mestre, professor, Department of Biomedical Sciences, Baker Institute for Animal Health
Q: What has been your path leading to Cornell?
I studied veterinary medicine at University of Sydney, Australia and had an interest in equine health right from the start. Over my degree, I had the opportunity to spend a summer at Cornell as part of the Leadership Program for Veterinary Students, and one at North Carolina State University, experiences that really shaped my curiosity for research and interest in the genetic and molecular basis of disease processes. After graduation, I worked in leading equine clinical practices in Australia and the United Kingdom that specialized in reproduction. After two years working with some excellent mentors, I realized research was where my heart was, so I relocated to Australia’s capital, Canberra, to a do a Ph.D. in molecular and cellular biology and immunology at the John Curtin School of Medical Research, Australian National University, under great supervisors, Drs. Mark Hulett and Chris Parish.
Following my Ph.D., I took up a postdoctoral position in the laboratory of Dr. Douglas Antczak at the Baker Institute for Animal Health at Cornell, where I consolidated my current interest in genetics, pregnancy immunobiology and offspring health. In 2007, I accepted a faculty position at the Royal Veterinary College, University of London, where I have been for the last 15 years as head of the Equine Pregnancy Laboratory. I’ve been actively involved in teaching reproductive biology and stud medicine to pre-clinical and clinical veterinary and biomedical students.
Q: What drew you to CVM?
Having spent time at Cornell as a trainee, when I was approached about my position I was immediately curious as I had always enjoyed the energy, pace and collaborative spirit of scientific research at College of Veterinary Medicine. During my visit last year, I really felt this spirit. I was also attracted to developments and relaunch of the Center for Reproductive Genomics, which is currently well aligned to the direction of my research, which aims to better understand genome instability in the placenta and its role in pregnancy loss.
Q: What is your clinical or scientific area of expertise?
My laboratory focuses on understanding the normal processes required to support a healthy pregnancy and delivery of a neonate programmed for lifelong health, as well as identifying the pathologies that compromise pregnancy, including those that are lethal. My wider goal is to support veterinarians to make evidence-based clinical decisions in reproductive medicine through improved diagnostics and treatments for pregnancy conditions, primarily in the mare, but also informing health strategies in humans and other veterinary species.
Q: What drew you into this area? Did you have specific experiences, mentors or influences that helped guide you?
Over the two breeding seasons I worked with Dr. Jane Axon at Scone Equine Hospital, I was exposed and contributed to the management of a huge caseload of foals, with up to 100 new neonate cases admitted monthly at peak times. At the time, we were focused on treating disease processes of neonatal life, but essentially those diseases resulted from pathologies that originated much earlier in embryonic and fetal life. Here started my fascination with the link between fetal and neonatal health and pathologies that lead to a pregnancy failing.
Q: What past professional work are you most proud of and why?
My proudest professional moments involve teaching and mentoring. I have had the great pleasure to teach and work with some fantastic veterinary and graduate students, both in my laboratory and as an academic tutor. Being part of their first ‘new discovery,’ conference abstract acceptance and/or manuscript acceptance is a real privilege.
Q: What about your clinical work, research or teaching innovations are you most excited for or proud of and why?
This is a hard question, as each research achievement builds on the shoulders of previous work in the group. Saying that, one achievement that spans multiple studies which I am proud of is our biobank of tissues from clinical cases of pregnancy loss that has allowed us to tackle a range of novel research questions around early pregnancy loss and abortion. Using this material, we recently found horse pregnancies fail due to aneuploidy, meaning the embryos possess an abnormal number of chromosomes. This accounted for 20% of cases of early pregnancy loss, and represented the most common cause of early pregnancy loss in the mare reported to date.
Q: What impacts or applications do you hope to see your work have on the world, or on human, animal or planetary health?
My long-term goal is for our studies of equine pregnancy to lead to evidence-based decision making in reproductive practice through the development of novel diagnostic tests and treatments for pathologies that compromise pregnancy and fetal health. Due to similarities in aspects of the biology of pregnancy in the mare and women, ultimately I hope our studies of horse pregnancy provide a natural disease model that also informs our understanding of the underlying mechanisms of miscarriage in women, a devasting condition for couples.
Q: What questions are you looking to answer next or areas you plan to explore?
Growth of the placenta is key to support of the developing fetus, but we still know very little of the processes that regulate its development. We will be studying the molecular mechanisms that control the development of trophoblast lineages in the equine placenta, as well as how these processes are disrupted in a compromised pregnancy. Related to this work, we are also investigating structural genetic variants and SNPs associated with fetal lethality. We have identified microdeletions and microduplications (loss and gain of small segments of chromosomes called copy number variants) that are associated with pregnancy loss. The role of CNVs in normal placental growth, as well as pregnancy failure, is poorly understood. We plan to characterize these CNVs in healthy and failing placentae. We are also interested in identifying variants that influence non-lethal conditions of the fetus such as growth restriction and congenital musculoskeletal disorders.
Q: What’s something most people don’t know about you?
I owned a racehorse in Australia with my family called ‘My Psychiatrist’ that had quite a following, mostly due to her name, not always her athletic talents!
Q: What’s the best part of being a clinician or scientist?
My passion is solving problems and in essence that is what we are doing day in and day out as a scientist. Sometimes that problem-solving can take years, which makes the day you find the solution even more satisfying!
Q: What’s the most challenging part?
Solving problems that take years of work also requires a lot of patience and perseverance!
Q: What are the benefits of working at CVM? At Cornell?
My research is at the interface of basic science and clinical research, and CVM provides a great combination of cutting-edge research that extends from molecular mechanisms to applied clinical practice. There is a real sense of collaboration when you meet people and there are excellent facilities available for our work. The established links to Weill Cornell Medicine also mean our work has the opportunity to have an impact beyond animals.