Direct Coombs Testing
A Coombs test is performed to detect the presence of antibody against red blood cells. The test is used to support the diagnosis of immune-mediated hemolytic anemia (IHA). Up to 66-75% of dogs with IHA will have a positive Coombs test. A Coombs test is indicated for animals with a regenerative or severe non-regenerative anemia, that have had other causes for the anemia (e.g. hemorrhage) ruled out. The Coombs' test has no diagnostic value in a non-anemic animal. Many animals with other diseases (e.g. infection, neoplasia) can have a positive Coombs test, but do not have IMHA. Therefore, a positive Coombs test in this setting is unlikely to be clinically relevant or diagnostic. Many people use a Coombs test for helping to confirm the diagnosis of SLE, however, hemolytic anemia is observed infrequently in SLE (13% in one study), and only 4% of dogs with SLE will have a positive Coombs test; indicating that this is a test of low yield in this setting.
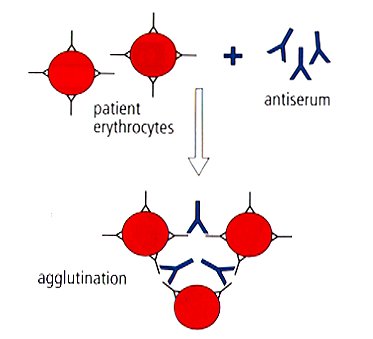
Anti-red cell antibodies are attached to the patient's erythrocytes. When the patient's blood is reacted with the Coombs reagent (antiserum), the antibodies in the Coombs reagent bind to the antibodies attached to the erythrocytes, causing agglutination.
At Cornell University, we perform a direct Coombs test. In this test, we are looking for antibody adhered to the patient's red blood cells. For this reason, we need red cells from the patient, preferably asEDTA-anticoagulated blood. The direct Coombs test is more sensitive than the indirect Coombs test, which assesses for antibody in the patient's serum to red cells. In some patients with IHA, all of their antibody may be attached to their red cells, therefore they may have a negative indirect Coombs test, but a positive direct Coombs test. In the Coombs test, washed red blood cells from the patient are incubated with the Coombs reagent at 37 C. The Coombs reagent is polyvalent and contains species-specific anti-IgG, anti-IgM and anti-C antibodies. If any of these are present on the patient's red blood cells, crosslinking will occur, which can be visualized microscopically as agglutination. We do perform dilutions of the Coombs reagent, in an effort to eliminate the prozone effect (a false negative reaction due to extremely large amounts of antibody in undiluted samples). Because the Coombs reagent must be species-specific, we only offer Coombs testing in dogs, cats and horses.
For samples submitted to the laboratory through the Animal Health Diagnostic Center, we request the submission of freshly prepared air-dried unstained blood smears, as well as EDTA blood. We always examine a peripheral blood smear with all our Coombs tests. In this way, we can provide additional information. For example, if the Coombs is negative, but we see a lot of spherocytes in the blood smear, an IHA is likely and we will add a comment to this effect. We have made many unsuspected diagnoses from examining blood smears submitted with Coombs tests, including acute leukemia and immune-mediated thrombocytopenia!! In most of these cases, the Coombs test result has been negative and blood smear examination provided diagnostic information for the case, whereas the Coombs test did not. Coombs tests should be performed as soon as possible after collection, so the sample should be shipped overnight, to reduce the numbers of false negatives or positives.
Our Coombs results are reported as negative or positive. We do not add a comment to the result, unless we see something untoward in the blood smear. We do not report a titer, because we are diluting Coombs reagent, not red blood cells. In addition, there are no published studies that indicate a titer provides additional diagnostic information. In some patients, a weak positive Coombs result occurs. We will flag these results, which indicate that the Coombs was positive at the lowest dilutions of the Coombs reagent. This type of result demonstrates that there are antibodies attached to the red blood cells, but does not confirm that the anemia is due to immune-mediated hemolysis (antibodies can attach to red blood cells in a variety of conditions, e.g. infectious diseases, but do not produce hemolysis or anemia). However, in some IHAs, especially non-regenerative forms, many dogs have weak positive Coombs titers. Some of these dogs do not have circulating spherocytes either.
Causes of positive reactions not associated with IMHA (false positives)
- Post-transfusio
- Non-specific coating of erythrocytes
- In vitro complement binding during storage
Causes of negative reactions in animals with IMHA (false negatives)
- Antibody present in too low a titer to be detected by the test
- Prior corticosteroid therapy (a positive Coombs' test would still be expected if the animal was still showing clinical signs of the anemia or there is evidence of ongoing hemolysis)
- Elution of a weakly bound antibody during washing
- Detachment of antibody or complement from erythrocytes due to sample aging


