Companion Animal Hospital
Ophthalmology
 The Ophthalmology Service at the Cornell University Hospital for Animals provides scheduled and emergency care for companion animals with eye and vision problems. Our staff include the board-certified ophthalmologists and residents who collaborate with other veterinarians across the Northeast to provide comprehensive eye care.
The Ophthalmology Service at the Cornell University Hospital for Animals provides scheduled and emergency care for companion animals with eye and vision problems. Our staff include the board-certified ophthalmologists and residents who collaborate with other veterinarians across the Northeast to provide comprehensive eye care.
Nutrition
The Cornell University Hospital for Animals is among a small number of animal hospitals across the nation that offers comprehensive nutrition services provided by boarded specialists in the area of veterinary nutrition for hospital and clinic patients, as well as nutrition consultations for animal owners across the country.
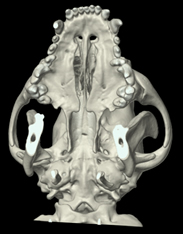
Imaging Service

The Imaging Service at the Cornell University Hospital for Animals takes pride in providing excellent patient care and customer service.
Emergency and Critical Care
The Emergency and Critical Care Service at the Cornell University Hospital for Animals provides evaluation, medical care and surgical treatment to severely injured or ill companion animals, as well as ongoing care for critically ill or injured animals 24 hours a day, 365 days a year.