“Fighting the good fight”: Alumni face off against a pandemic
By Melanie Greaver Cordova

A workbook on one coffee table, some markers and paper on another. A young boy sits cross-legged reading a book while a young woman helps a girl with her math homework. This isn’t a pre-coronavirus classroom — this is the reception area to Davis Companion Animal Hospital, a veterinary practice in Connecticut run by Brad Davis, D.V.M. ’83. To help his team adapt to the surreal new reality of working during a pandemic, he’s transformed his client waiting area into a daycare and classroom for their children.
“Several of my technicians and staff have young kids, and there was just no daycare or even school for them,” says Davis. He also hired one of the technicians’ daughters to teach kids who needed more guided instruction. “They’re all out in reception — teaching the kids and doing their own homework, too.”
Transforming office space is just one of the many singular adaptations Davis and other alumni of the Cornell College of Veterinary Medicine (CVM) have made to ensure that their teams, businesses and patients continue to receive the attention they need despite a global pandemic that shut down most of the United States mid-March.
New processes, new challenges

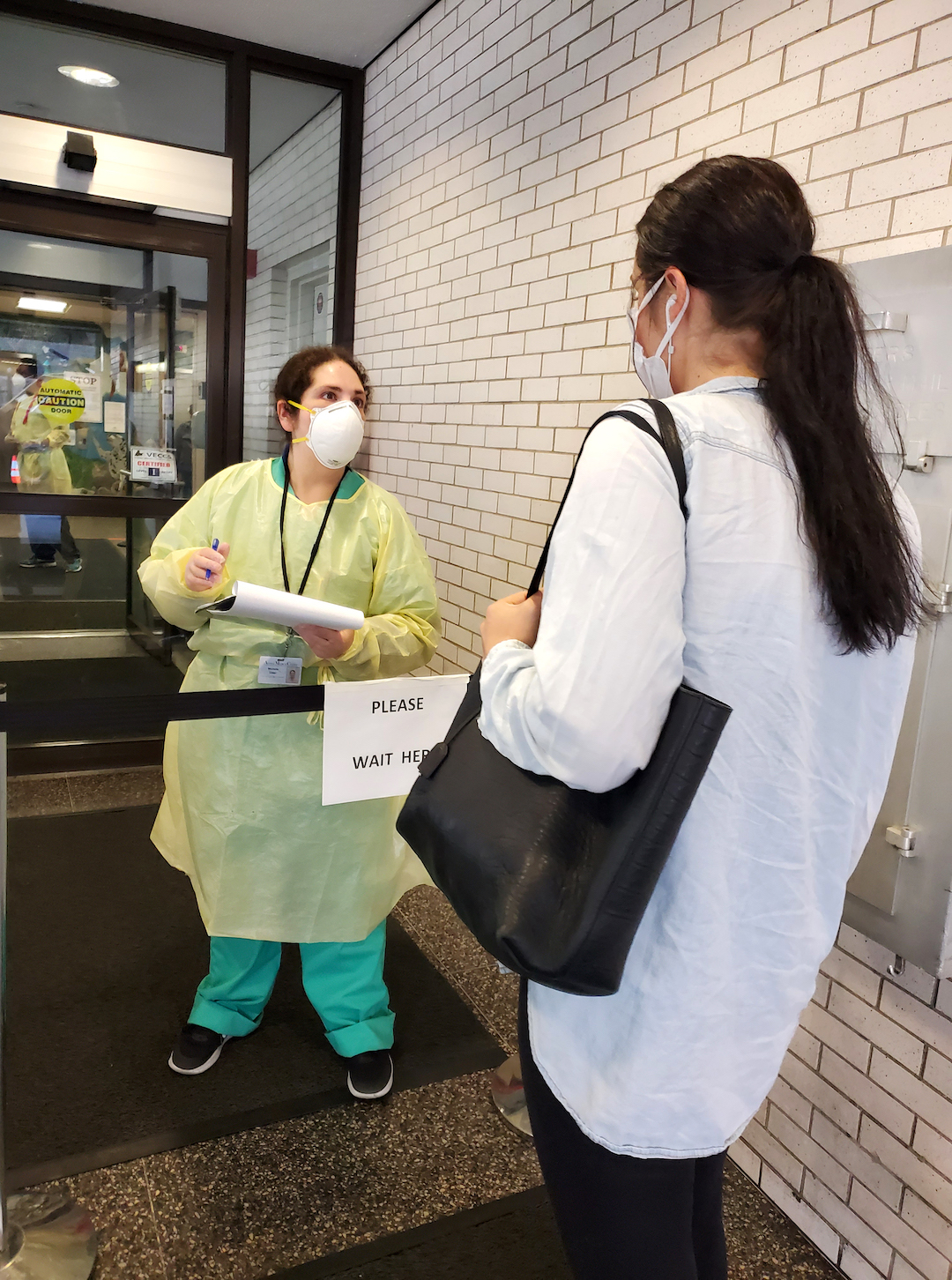
As soon as state and local governments issued shutdown orders in an attempt to mitigate the spread of the coronavirus, veterinary alumni across the country pondered a litany of questions about how this would affect their teams, patients and businesses. The first hurdle was handling the logistics. Many small animal practices, for example, transitioned to curbside or parking lot drop-off and pick-ups. This was the case for Ann Hohenhaus, D.V.M. ’85, staff doctor in oncology at the Animal Medical Center (AMC) in New York City — a early hotspot for the virus.
“The problem with being in New York City is that we don’t have a lot of space,” says Hohenhaus. “Our parking lot has tents where clients can wait, but when we get into summer and it’s 95 degrees, at some point they’ll get heat stroke.”
She notes that there’s just not enough room in the hospital for the social distancing required to keep everyone safe. “It’s all a work in progress, and when they can’t wait outside it’ll add another layer of difficulty.”
The Maryland Veterinary Group, an equine practice owned by Nicholas Meittinis ’85, D.V.M. ’89, predominately serves racehorses. When the pandemic hit, they immediately put social distancing protocols in place and adjusted their overall approach. For example, grooms became the horses’ primary handlers so the technicians could stay at home. “We also have a bookkeeper who would usually be working at the track, but now she’s working from home, too,” says Meittinis.
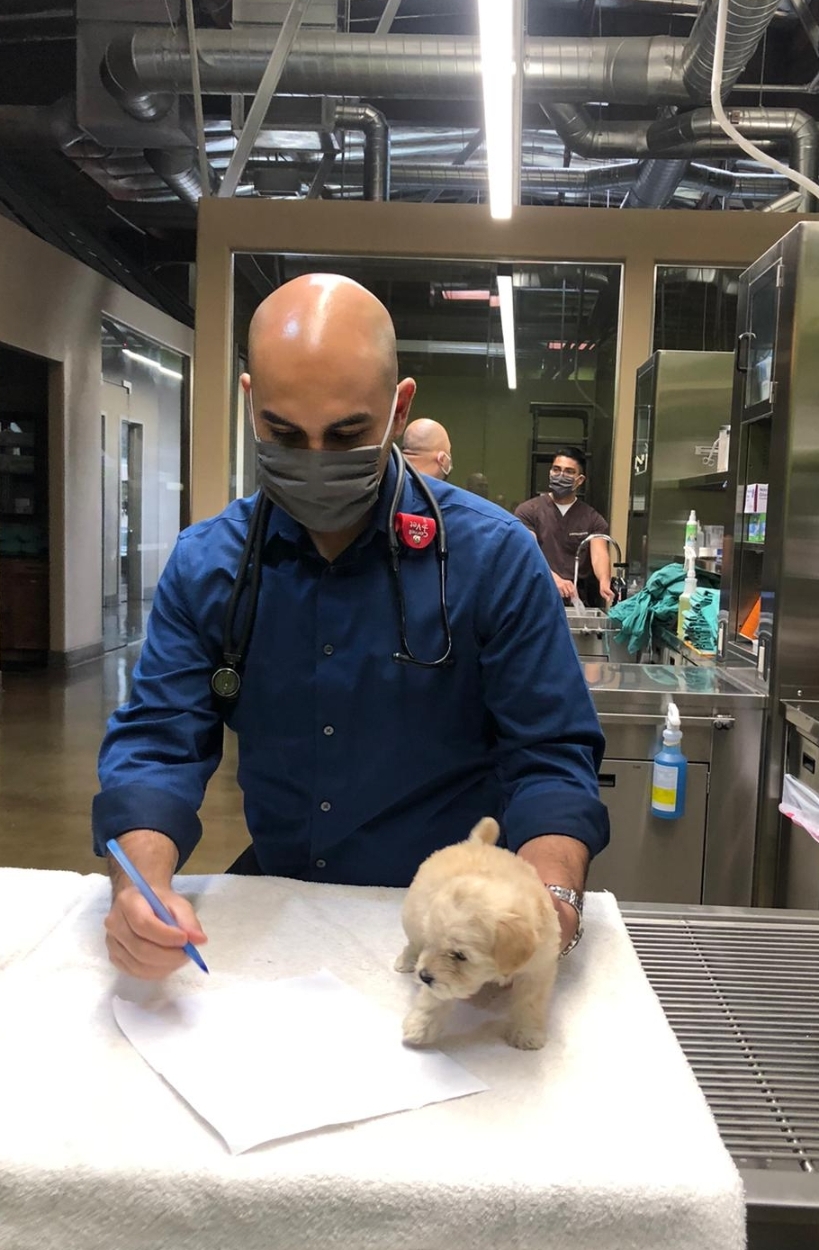
West Coast practices similarly altered their processes. “Since clients aren’t allowed in the hospital, the biggest change has been implementing our parking lot service,” says Julio Lopez, D.V.M. ’08, medical director at the Veterinary Care Center in Los Angeles. Consequently, the usual back and forth that happens during an exam is no longer as easy, he says, as they have to rely on phone communication. But even that comes with its own logistical hurdles, adds Davis.
“What we found out right away with our curbside service was that simply communicating with clients was challenging,” Davis says. “We only had five phone lines into the clinic, but one’s tied up with the credit card machine, and at times it just wasn’t enough.” He came up with a two-pronged solution to address this by purchasing a batch of internet-based phones and by hiring a “runner” who goes out to clients’ cars as they arrive — following social distancing and mask requirements — to help them check in. “She’s eliminated half the need for phone lines on her own,” he says.
Indeed, these unusual adaptations were at times so stark that Hohenhaus notes she sometimes feels like she’s entered a whole new profession. With new policies changing so rapidly, usually in the interest of improving efficiency or safety measures, “it’s like working in a brand-new job,” she says. Not seeing clients face-to-face in particular has been a paradigm shift. “I’m taking care of the pets of people whom I’ve never met, which is weird,” says Hohenhaus. “I could walk past them on the street and not even recognize them.”
For Jennifer Koga ’84, D.V.M. ’88, who is a veterinarian at a large, 24-hour general practice in Los Altos, California, her workplace reduced services to only emergency or urgent cases — like many veterinary hospitals, Cornell’s included. Their doctors’ schedules also changed, sometimes inconsistently, based on need. To adapt, her team created a “Dr. Coronavirus” category in their software. “One doctor was assigned each day to be Dr. Coronavirus,” says Koga. “This doctor is responsible for contacting owners with lab work results from the previous day, doing call-backs, approving prescription refill request from clients and so on.” This master-of-all-trades role has greatly helped their transition, notes Koga, as have their video visits with clients.
People’s desire for high-quality care for their pets did not wane during the pandemic. If a pet needs surgery or chemotherapy, owners will want them to have it, says Hohenhaus. “That’s one reason why AMC hasn’t closed, because we’re doing what helps pets,” she says.
For Meittinis, his team of six was similarly still providing veterinary care to horses, though with less frequency. “It felt like things came to a halt,” he says, “because all racing was canceled for several weeks. That doesn’t mean the horses don’t get sick, only that they weren’t asking us to examine them as often since they had to be mindful of reduced finances.”

Emotional, financial challenges
In the interest of helping pets and owners during such trying times, veterinarians have struggled with how to approach part of the job that is already an emotional challenge: euthanasia.
“While clients aren’t allowed in the hospital, we do make exceptions when it comes to humane euthanasia,” says Lopez. “As long as the pet owners are not experiencing any symptoms of COVID-19, they can be present, given all that is involved with that decision.”
Koga’s hospital also allows family members into the facility for such a situation. “But only two people can be present at a time, and our staff is in full personal protective equipment for all euthanasia procedures,” she notes.
The team at Davis Companion Animal Hospital has tried to find a middle ground, where part of this procedure can happen on a nearby picnic table set up beneath a large maple tree so the family can be with the pet while the sedative is administered, and then the pet is taken inside for the rest of the procedure. No matter what, notes Hohenhaus, such considerations complicate an already fraught decision. “When we talk to the owners over the phone about their pet’s condition, they aren’t there in the exam room to see their poor or deteriorating condition. They don’t get the full picture and it’s hard to convey such things over the phone,” she says.
These logistical questions are hard enough — the safety of clients and staff could be at stake, but so could the veterinarians’ livelihoods. The financial ramifications of a statewide shutdown of nonessential businesses, and a necessary reduction in services, affected these practices despite being considered an essential service. Koga describes how she voluntarily didn’t take a paycheck for either April or May to help the hospital, and worked as a client service representative on her days off. “We had to put half our doctors on furlough every other week, alternating with the other half,” she said. “I only worked when they needed another doctor on particularly busy days.”
This reduction doesn’t necessarily mean there was no work to be done. For some it was quite the opposite. Often it was more of a consideration of density, and knowing that the virus spread more easily based on proximity and duration of exposure.
“I considered splitting the team in half to support the hospital and maintain a level of care that was appropriate,” says Davis. “Ultimately, we made the hard decision that we were just going to continue as-is. We needed everyone to work because the caseload remained so high.”
His team committed to extreme caution and together discussed areas of risk and exposure both at work and at home. “We knew we were only as healthy as the weakest link in the chain and everybody took it very seriously.” This way, through caution, workers kept their hours consistent. Davis also took advantage of the Paycheck Protection Act, using these funds as a buffer and to help with taxes.

Universal struggles
Not all veterinary professionals are in a clinical setting, of course. For Andrew Di Salvo, D.V.M. ’15, his work as the wildlife veterinarian for the state of Pennsylvania often had him in the field. But such activities have been limited since early March, and Di Salvo went from reporting to his office in Harrisburg to working from home.
“It’s unfortunate because field activities are a welcome change of pace from the office environment,” he says. Even working remotely, he still assists with tasks like developing the wildlife health database system, providing consults to colleagues, conducting wildlife health and chemical immobilization trainings for biologists and wardens, coordinating surveillance efforts, generating wildlife disease response plans and so on. He’s also leading the wildlife health protocol development for new and emerging diseases that may affect wildlife — such as SARS-CoV-2 and the current outbreak of rabbit hemorrhagic disease virus 2 in the Southwestern United States.

With so much work still to be done, the lack of face-time with colleagues is challenging. “Humans are social creatures and I do miss the day-to-day interactions with my colleagues and the sense of camaraderie that develops as a result of working all within the same building,” says Di Salvo. Even so, technology has been a huge component to keeping things running. “Much of my days are spent on phone and video conference calls,” he says.
This struggle extends even to the clinical space. Says Hohenhaus, “My life revolves around cords these days.”
Koga’s team was able to reopen their satellite clinic in June, and has incorporated tech solutions there by using a live Zoom video feed in the exam room that a client can connect to while waiting in the car. “We can then interact with the owner during the exam, and the owner can watch the physical exam,” she says.
Professionally prepared
While there have been unprecedented challenges in the current pandemic, these alumni found that their veterinary training prepared them in ways both expected and unexpected. Regarding the expected, Koga for example knew that her infectious disease training and knowledge of biosecurity that came with her education and practice would be a boon in such times.
“Veterinarians have been very well trained on the prevention and spread of infectious disease,” she says.
Hohenhaus agrees. “For biosecurity, you know to touch as little as possible, and you really think, ‘Do I need to touch this? Can I send this remotely instead of printing and handing it off myself?’” She notes that it’s not just the content of the training, but also the method: Veterinarians are trained to be problem-solvers, and that’s been crucial when adapting — especially to life in a very altered New York City, for one.
“Our multi-species training is probably the impetus for flexible thinking,” Hohenhaus says. “Maybe you have a species you’ve never seen before, or a problem you haven’t seen before in an animal you’re familiar with. You have to adapt what you know. That’s an important trait.”
Meittinis suggests that veterinary training indeed has broad applications: “I want people to know that, yes, they can turn to their veterinarian for advice regarding viral illnesses of this sort.”
For Di Salvo, it was the time spent in relative isolation in previous positions — conducting sea turtle research on a secluded beach in the Galapagos Islands and working as a veterinarian in rural Namibia — that has proven unexpectedly familiar. “I’ve worked in remote locations before and I feel like that’s prepared me well for what’s going on now,” he says. “The sense of isolation is very similar.”

Projecting empathy
In some ways, the stressors of veterinary work before the pandemic hit have now intensified. This certainly includes the financial concerns of an unpredictable economy paired with risk-averse clientele — but factors like compassion fatigue and client education are also top of mind. Davis has observed that he must make sure he’s addressing people’s concerns quickly and in detail, even more so than usual, simply because a connection with clients is lost in not seeing them in the exam room. “This may be the new normal,” Davis says. “You have to find ways to project empathy and let people know that you really do understand their worries. Even having your face covered when you do come into contact with people creates a barrier that’s difficult to deal with.”
Additionally, for Davis, client education has at times extended to pandemic basics: Wear a mask, wash your hands and keep your distance. “We try to keep clear communication about the process and tell them nicely they’re required to wear a mask,” Davis says. “We explain the virology of the virus for some people who just don’t understand, who resist it.” Everyone is also learning new social skills, he notes. “How do you pull away from somebody without insulting them?”
Di Salvo agrees that some of these challenges are intensifying what is already a challenging component of veterinary work, but hopes the ultimate outcome is positive. “I’m hopeful that our collective experience during these trying times will reinforce an appreciation of the essential work veterinarians do and garner more empathy from the public moving forward,” he says.
Building a bond
One of the challenging things to maintain during the coronavirus pandemic is a bond with clients. Other clinical veterinarians echo the same body language concerns Davis has raised. Says Lopez, “Pet owners are giving us a tremendous amount of trust, given they can’t see how we’re interacting with their pet or how thorough of an exam we’ve done. We also lose the ability to read body language, which is very important in helping guide conversations.” Without the in-person interaction, it is more difficult to build that crucial bond with clients.
As a cancer specialist, Hohenhaus has always relied on body language to determine if a client might, for example, suddenly burst into tears when hearing bad news. “I find it very difficult on the telephone,” she says. “Some of my colleagues are using more texting, but you can’t use a text message to tell someone their pet has cancer, that it’s spreading and they’re about to die.” She adds that she misses her regular clients, that the bonds she’s made has turned them into friends. “As much as I miss the pets I take care of, I miss the people, too.”
This is actually one of the reasons Davis has held off on incorporating telemedicine into his practice. “I got into this profession because we had the ability to bring the patients and their owners into the clinic,” he says. “Telemedicine might just increase the divide.”
He notes that sticking with in-person visits has not diminished his hospital’s productivity, as he might have expected. “My staff are actually telling me that I’m more efficient,” he jokes. “I’m seeing more patients; most of these owners I’ve known for decades, so I tend to get chatty. I know them like family. I can’t do that right now.”
Although there might be fewer “chatty” visits, there is an efficiency tradeoff in other ways. Things can simply move faster when an owner is present, says Koga. “It is very hard to be efficient when the owner can’t even come into the building,” she says.
Hohenhaus seconds this, noting that the constant calls between doctor and patient, and the new policies and safety procedures, can eat up a lot of time. All agree, however, that while they must adjust to the new normal, there’s not one way to do so. Some approaches certainly are tech-based. Hohenhaus, for example, had time away scheduled to give lectures at a meeting. “Instead I gave them from the bedroom,” she says. And Di Salvo, limited to working from home instead of in the field, jokes, “If you know of a work-around that could cut down on the number of emails I need to read and reply to, I’m all ears.”
Some adjustments are exacerbating existing professional concerns, but the desire to help patients remains a constant. “The best example for me, “says Davis, “is pulling into work one morning and seeing my associate veterinarian standing next to a car and advising a client in the pouring rain. The dedication is real.”
Meittinis has seen also this dedication among his team, but more importantly among his clients. “I’m proud of them. They’ve understood the ramifications of exposing us to certain dangers,” he says. “They’re more selective for what they call us in for. It’s a good reminder that we’re all in this horse business together. We look out for each other.”
Staying plugged in

The internet has made it possible for people to stay connected despite the physical distance between them. It has also served as a point of connection for these veterinary professionals. Hohenhaus notes that the regular meetings hosted by the Cornell University Hospital for Animals over Zoom during the pandemic have helped her keep in touch. “I’ve often wondered what the pandemic would be like if we didn’t have the internet,” she says. Additionally, Hohenhaus attended Cornell’s first-ever Virtual Reunion, even though she was disappointed that the in-person gatherings were canceled.
“That was one of the worst weeks during the pandemic,” she says. “It was my 35th Reunion, everything was canceled, but Saturday night we had a Zoom conference, and I got to see so many children, grandkids and kids we probably wouldn’t have gotten to meet in person. So that was fun and unexpected.”
Koga has seen similar innovative uses of the internet to stay connected and help one another. Her team has used Zoom for doctor meetings to go over protocols and touch base, and “one of our veterinarians started a private Facebook group for our staff, where we can share uplifting stories, videos, memes and so on.”
The blend of information-sharing and personal support is something Di Salvo has also seen. He says he checks in with his closest colleagues multiple times a week and they often commiserate over the changing world. Adds Di Salvo, “I think I’ve come to more appreciate the value of daily interpersonal relationships, and I’ve developed a stronger understanding of what’s important in life.”
Ultimately, what keeps Davis going is his professional mission: taking care of patients. “I think that veterinary teams are fundamentally empathetic, so it’s a challenge for people to absorb the additional stress,” says Davis. “Just caring for the dogs and cats that come in, that’s the most cathartic thing we can do, you know? Fixing something that is broken is always worthwhile.”
Lopez agrees. “Companion animals are very important parts of our lives, especially during these times, and we have to be there for pets when they need us.”
A slow transition

When the pandemic wanes and certain parts of the country are cleared to reopen fully, veterinary professionals will be faced with a challenging question: How do we transition back to our “normal” jobs? For some, it might mean refiguring exam rooms to accommodate social distancing precautions. For others, like Meittinis, it might mean simply catching up on all the regular visits missed during the months when non-emergent cases were postponed. “We’re at twice the caseload just to catch up,” he says. “We’re grateful to be able to work on animals and know they’re an important part of our lives.” He notes that the pandemic has made him re-evaluate his off-work life as well, the faint silver lining to the pandemic being that he could more fully focus on life at home.
Indeed, for some a transition to normal might mean enriching personal lives with travel and entertainment that was previously canceled so that work-life balance is easier to maintain as things ramp up.
“When will I be comfortable going to a Yankees game with 43 thousand people?” asks Hohenhaus. “Or riding like a sardine in a subway car on the way home?”
This will almost certainly depend on reliable testing and a vaccine for coronavirus. “Global access to highly-sensitive and highly-specific diagnostic tests and an efficacious vaccine are the most important factors when it comes to reopening and returning to any semblance of ‘normal,’” says Di Salvo. “Things will never be exactly the same and our country must adapt to be more prepared for the next pandemic.”
“One of the most important factors is for the number of hospitalizations to go down,” says Meittinis.
This hits home especially for Hohenhaus, who saw over 800 of her fellow New Yorkers dying each day during the height of the pandemic. “Terrible,” she says. “It was terrible. I’m hoping that never happens again. It’s a reasonable wish to stay healthy.”
This desire is echoed by alumni across the country, who make reasonable precautions in their daily activities, managing to care for animals despite a global pandemic. “I think our staff has done an amazing job in caring for our patients during a very stressful time,” says Koga. “I am very proud of the people at our facilities.” It will be a slow process to fully recover, she says, but they’re ready to put the work in.
“I’ve seen and heard of so many great examples of selflessness, empathy and courage during this pandemic,” agrees Di Salvo. “So many have risen to the challenge and it’s nice to be reminded that there are good people out there fighting the good fight.”
While the nuts and bolts of the veterinary field may never be the same, the high degree of adaptability and professionalism of CVM alumni is a constant. Time and again, they’ve shown that they’re prepared to face the world’s most pressing problems with integrity, using the strength of their training — both at Cornell and at work in the world — to forge a resilient future. •



