Vitamin K Deficiency
Overview
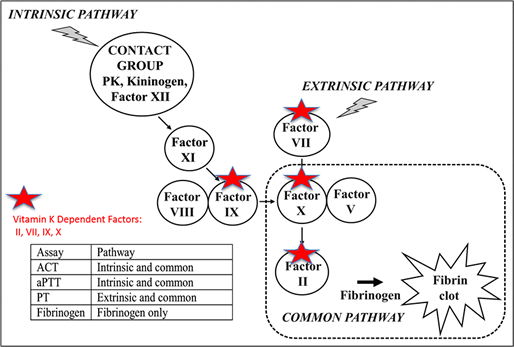
Vitamin K is a fat-soluble vitamin essential for the post-translational processing of the prothrombin group of coagulation factors (Factors II, VII, IX, and X). Vitamin K deficiency causes excessive bleeding due to failure of normal fibrin clot formation. Clinical signs of bleeding depend on duration and severity of vitamin K deficiency and include prolonged bleeding from minor wounds, spontaneous hematoma formation, intracavitary hemorrhage, and death due to blood loss and acute hemorrhagic shock. Anticoagulant rodenticide poisoning is the most common cause of severe, acute vitamin K deficiency in dogs and cats.

Severe SQ bleeding in a dog caused by vitamin K antagonism (anticoagulant rat poison toxicity).
Vitamin K Metabolism and Actions
Vitamin K Absorption and Recycling
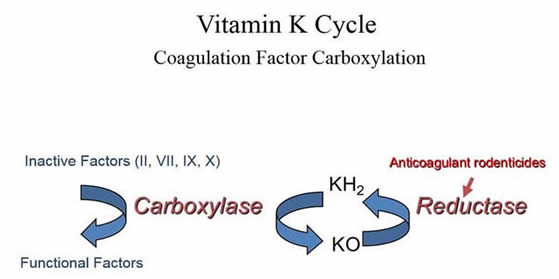
Dietary Vitamin K1 (phylloquinone) is high in green leafy plants. Vitamin K2 (menaquinone) is also produced by fermentation and gut microbiota. As a fat-soluble vitamin, Vitamin K is absorbed after bile salt and pancreatic-dependent solubilization and uptake of lipid micelles into enterocytes. After intestinal uptake, Vitamin K undergoes intra-hepatic recycling where it acts as a cofactor for post-translational carboxylation of vitamin K-dependent proteins. Vitamin K participates in these reactions through oxidation of vitamin K hydroquinone (KH2) to vitamin K epoxide (KO). The KO form of vitamin K is continually recycled to replenish KH2 by the enzyme KO reductase.
Vitamin K-Dependent Proteins
The glutamate residues on proteins that undergo vitamin K-dependent carboxylation are referred to as “Gla-domain” and the group of proteins that undergo this modification, including coagulation factors, are known as “Gla proteins”. The Gla residues on these proteins are required for protein interaction with calcium. In addition to intra-hepatic modification, some Gla proteins undergo vitamin K-dependent carboxylation in the vasculature. Severe Vitamin K deficiency manifests clinically as a bleeding diathesis, however vitamin K is required for functional activity of additional proteins with a variety of physiologic roles.
-
Circulating Gla domain hemostatic proteins
- Procoagulant coagulation factors: Factors II, VII, IX, and X
- Anticoagulant factors: Protein C, Protein S, Protein Z
-
Tissue and vascular Gla domain proteins
- Bone metabolism, cell migration: Osteocalcin, Periostin, MGP(matrix Gla protein),
- Vascular smooth muscle function, cell proliferation: MGP, Gas6 (growth arrest specific protein-6)
Diagnosis of Vitamin K-dependent Coagulopathy
Coagulation Tests and Sample requirements
Coagulation screening tests and specific assay of the vitamin K-dependent coagulation factors are direct measures of the cause of bleeding in vitamin K deficiency states. Citrate plasma, drawn antemortem, is the only acceptable specimen-type for these assays. See links for more sampling information and the Vitamin K-Deficiency panel.
-
Coagulation Screening Tests: (aPTT, PT, TCT, fibrinogen)
The PT is the most sensitive screening test to detect early or mild vitamin K deficiency, however patients actively bleeding due to vitamin K deficiency have prolonged PT and prolonged aPTT. Fibrinogen and the TCT screening test are normal in vitamin K deficiency states. The characteristic pattern of vitamin K deficiency is therefore normal fibrinogen, but marked prolongation of PT and aPTT. -
Specific Factor Assays
Due to coagulation Factor VII’s short plasma half-life (approximately 7 hours), Factor VII deficiency develops early in the course of a vitamin K deficiency state. Sensitive PT assays will be prolonged as Factor VII activity falls below 30 to 40% of normal. Clinically severe bleeding develops as all the vitamin K-dependent factors decrease. The finding of combined deficiency of these Factors (Factors II, VII, IX, and X), but normal fibrinogen (not vitamin K-dependent) is the hallmark of vitamin K-dependent coagulopathy. Protein C is an additional vitamin K-dependent hemostatic protein with very short half-life whose levels are markedly decreased early in vitamin K deficiency states. -
Response to therapy
Replacement therapy with Vitamin K1 (phytonadione at 2 to 4 mg/kg/day) will correct coagulopathy over the course of 12 to 24 hours from initiation of therapy. Samples to document vitamin K-dependent coagulopathy, therefore, should be drawn before (or within 6 hours) of the first dose. Measurement of the PT and/or Factor VII on paired pre-treatment and 24 hours post-treatment samples can be used to diagnose vitamin K-dependent coagulopathy and confirm appropriate response to treatment. See treatment information.
Vitamin K Deficiency Disease Differentials
-
Vitamin K Absorption Defects
- Intrahepatic cholestasis
- Biliary obstruction
- Chronic oral antibiotic administration
- Infiltrative bowel disease
- Dietary vitamin K deficiency
-
Vitamin K Recycling Defects
- Anticoagulant rodenticide toxicity
- Dicoumarol (moldy feed) poisoning
- Coumadin therapy
- Neonatal vitamin K deficiency
- Hereditary hepatic recycling enzyme defects (epoxide reductase or carboxylase defects)
Anticoagulant and Non-anticoagulant Rodenticides
Anticoagulant Rodenticide Toxicity
Anticoagulant rodenticides act by blocking hepatic vitamin K recycling (see image above). Ingestion of these products by pet dogs and cats is very common and consistently in the top 10 calls to the ASPCA poison control center. New federal regulations on the sale of these poisons are aimed at reducing exposures of pets and wildlife. Many products will remain widely available, however, and early recognition and treatment with Vitamin K1 are critical for successful management.
Management Protocol
- Identify the poison: brodifacoum, bromadiolone, chlorophacinone, diphacinone, indandione, and pindone. are all long-acting vitamin K antagonists. Warfarin is the only short-acting poison (1 week duration).
- Draw pre-treatment samples for coagulation testing before initiating vitamin K therapy.
- Treat for vitamin K deficiency pending initial work-up-many patients will have no known exposure.
- Induce vomiting if poison was ingested within 1 to 3 hours. DO NOT induce vomiting if the patient is bleeding.
- Transfuse (fresh whole blood, fresh frozen plasma, cryosupernatant) for immediate replacement of active factors. Transfusion is indicated for patients with signs of respiratory distress or severe blood loss anemia. The combination of fresh frozen plasma and packed cells is equivalent to fresh whole blood. See transfusion guidelines.
- Start with parenteral (SQ) injection of Vitamin K1 at 2.2 mg/kg, or oral therapy at the same dose. Use a tapering oral dosage schedule (reduce dose by one half q. 2 week) for a total of 6 to 8 weeks for patients poisoned by long-acting or unidentified products.
- Measurement of PT and/or Factor VII activity after 48 hours of discontinuing vitamin K can be performed to confirm resolution of vitamin K deficiency.
Non-anticoagulant Rodenticides
Some rodenticides in home and commercial use have no anticoagulant action. These products include bromethalin (neurotoxin), cholecalciferol (hypercalcemic renal failure) and zinc phosphide (phosphine gas induced pulmonary edema). Coagulation testing will NOT identify these toxicities and Vitamin K is NOT indicated in the management of these poisons. See Toxicology for additional information on diagnosis and treatment.
Links
- Vitamin K Deficiency Coagulation Panel
- eClin Path Vitamin K
- Animal Poison Control
- VSPN Network
- Society of Environmental Toxicology and Chemistry
- United States Environmental Protection Agency Rodenticide Information
References
- Brooks MB and DeLaforcade. Acquired coagulopathies In: Weiss DJ, Wardrop KJ (eds) 6th Edition Schalm’s Veterinary Hematology. Ames, Wiley -Blackwell, 2010: 654-660.
- Center SA. Diseases of the gallbladder and biliary tree. Vet Clin North Am Small Anim Pract. 2009 May;39(3):543-98.
- Center SA. Feline hepatic lipidosis. Vet Clin North Am Small Anim Pract. 2005 Jan;35(1):225-69. Review. PubMed PMID: 15627635.
- DeClementi C, Sobczak BR. Common rodenticide toxicoses in small animals. Vet Clin North Am Small Anim Pract. 2012 Mar;42(2):349
- Istvan SA, Marks SL, Murphy LA, Dorman DC. Evaluation of a point-of-care anticoagulant rodenticide test for dogs. J Vet Emerg Crit Care (San Antonio). 2014 Mar-Apr;24(2):168-73.
- Lisciandro SC, Hohenhaus A, Brooks M. Coagulation abnormalities in 22 cats with naturally occurring liver disease. J Vet Intern Med. 1998 Mar-Apr;12(2):71-5.
- Littlewood JD, Shaw SC, Coombes LM. Vitamin K-dependent coagulopathy in a British Devon rex cat. J Small Anim Pract. 1995 Mar;36(3):115-8.
- Mason DJ, Abrams-Ogg A, Allen D, Gentry PA, Gadd KR. Vitamin K-dependent coagulopathy in a black Labrador Retriever. J Vet Intern Med. 2002 Jul-Aug;16(4):485-8.
- Mayhew PD, Savigny MR, Otto CM, Brown DC, Brooks MB, Bentley AM, Runge JJ, Callan MB. Evaluation of coagulation in dogs with partial or complete extrahepatic biliary tract obstruction by means of thromboelastography. J Am Vet Med Assoc. 2013 Mar 15;242(6):778-85.
- Rattner BA, Lazarus RS, Elliott JE, Shore RF, van den Brink N. Adverse outcome pathway and risks of anticoagulant rodenticides to predatory wildlife. Environ Sci Technol. 2014;48(15):8433-45.
- Waddell LS, Poppenga RH, Drobatz KJ. Anticoagulant rodenticide screening in dogs: 123 cases (1996-2003). J Am Vet Med Assoc. 2013 Feb 15;242(4):516-21.
Frequently Asked Questions
- What sample type is required for the Vitamin K Deficiency Coagulation Panel?
- Can I submit post-mortem blood, tissue, or feed samples?
- What is the turnaround time and cost for the Vitamin K Deficiency Coagulation Panel?
- Is anticoagulant rodenticide toxicity a common cause of Vitamin K Deficiency?
- How long after ingestion of anticoagulant rodenticide (rat poison) will signs of bleeding develop?
- Will the Vitamin K deficiency coagulation panel detect non-anticoagulant rodenticides?
- What other diseases cause Vitamin K deficiency?
- Can I use the Vitamin K deficiency coagulation panel to screen for hereditary Factor VII deficiency?
What sample is required for Vitamin K Deficiency Coagulation Panel?
Separated citrate plasma (plasma from a blue top tube) is the only valid sample. DO NOT SUBMIT SERUM. Request test code COAGKDEF and ship at least 0.5 mL plasma in an insulated box with cold packs for overnight delivery. See Comparative Coagulation Sampling Overview for detailed sampling instructions.
Can I submit post-mortem blood, tissue, or feed samples?
No, coagulation testing requires citrate plasma drawn antemortem. For other sample types, use the test code ACOAGSOL to screen for the presence of specific anticoagulant rodenticide compounds in solids (tissue, feed) or test code ACOAGLIQ for submission of liquids (stomach contents, urine, post-mortem blood). Refer to the Toxicology test menu for more details.
What is the turnaround time and cost for Vitamin K Deficiency Coagulation Panel?
Vitamin K deficiency coagulation panels are performed daily (Monday thru Friday) and results reported within 24 hours of sample receipt. Refer to the AHDC test/fee list for current pricing.
Is anticoagulant rodenticide toxicity a common cause of Vitamin K Deficiency?
Yes! The ASPCA poison control center consistently lists rodenticides in their top 10 toxin exposures for domestic dogs and cats. Anticoagulant poisoning is one of the most severe acquired bleeding disorders diagnosed at the Comparative Coagulation laboratory. All species are at risk if they ingest the poisons, including cats or predatory birds that ingest rodenticide-poisoned prey.
How long after ingestion of anticoagulant rodenticide will signs of bleeding develop?
Anticoagulant rodenticides cause bleeding after a delay of at least 12 to 24 hours from the time of ingestion. These products block hepatic vitamin K recycling resulting in gradual depletion of circulating levels of functional coagulation factors (Factors II, VII, IX, and X). The type and amount of product ingested will influence the severity, onset, and duration of clinical signs.
Will the Vitamin K deficiency coagulation panel detect non-anticoagulant rodenticides?
No. Other rodenticides have different mechanisms of action. These products include bromethalin (neurotoxin), cholecalciferol (hypercalcemic renal failure) and zinc phosphide (phosphine gas induced pulmonary edema). The Vitamin K deficiency panel will identify patients with active bleeding due to anticoagulant rodenticides such as warfarin, diphacinone, and brodifacoum, whose mechanism of action is based on vitamin K antagonism.
What other diseases cause Vitamin K deficiency?
Vitamin K deficiency may develop in patients with biliary obstruction, liver disease, prolonged oral antibiotic therapy, and malabsorption syndromes. Screening to detect early deficiencies and vitamin K1 supplementation as needed will prevent bleeding complications if surgery or invasive procedures are performed.
Can I use the Vitamin K deficiency coagulation panel to screen for hereditary Factor VII deficiency?
Yes. Hereditary Factor VII deficiency causes specific prolongation of the PT assay and low Factor VII activity. In contrast to vitamin K deficiency states, the aPTT and all other factors are normal. Hereditary Factor VII deficiency has been well characterized in Beagles and Alaskan Klee Kai dogs, and isolated cases have been identified in several other canine breeds and in domestic cats.